Thalassemia treatment using umbilical stem cells
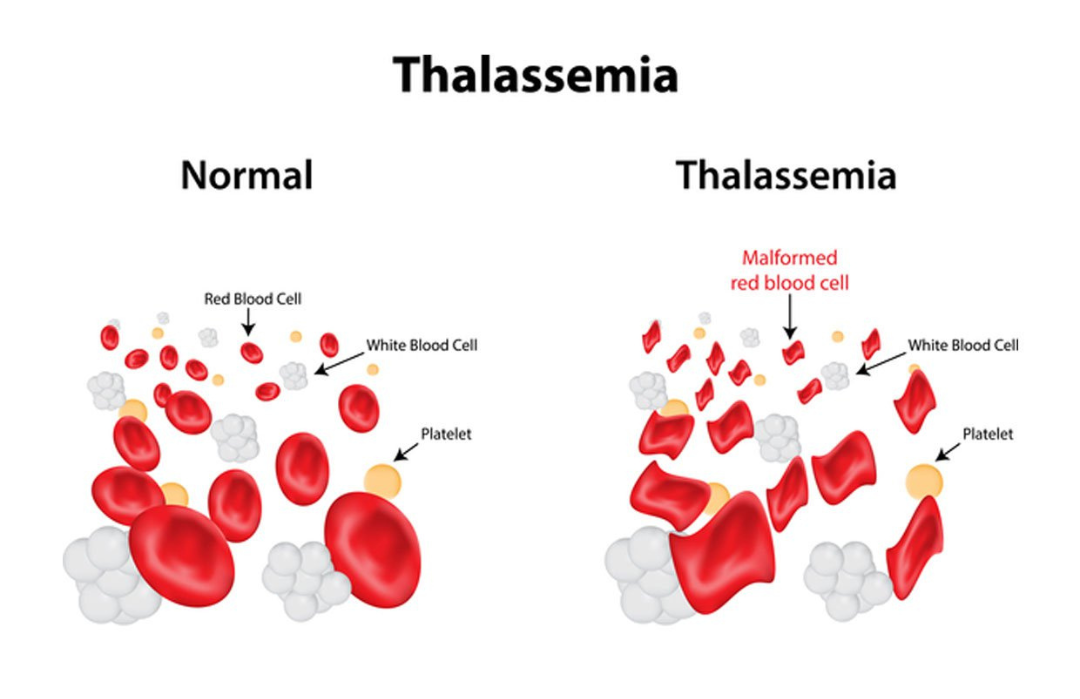
Thalassemia is a genetic hemolytic anemia. The disease mechanism affects the synthesis of globin chains in patients [1,2]. The cause of thalassemia is the unbalanced production of globin chains, resulting in ineffective erythropoiesis and increased hemolysis. While the carrier of the gene may not have symptoms, patients with severe thalassemia require regular blood transfusions and iron chelation to stay alive. The burden of the disease is enormous. One treatment is hematopoietic stem cell therapy. This method has brought significant results to patients with thalassemia and improved quality of life.
Thalassemia treatment methods
The traditional approach is conservative, with blood transfusions and iron chelation. This method transforms thalassemia into a chronic disease with a longer life expectancy. However, it leaves patients with a significant disease burden for a lifetime. Hematopoietic stem cell transplantation therapy is advocated for suitable patients. Understanding the mechanism of the disease is gradually opening up many prospects for cell therapy [3]. There are still many areas in the world that have not had access to this advanced method because of limited medical resources, leading to most patients living in those areas not being served.
Treatment of thalassemia with stem cells
Over the past 30 years, stem cell transplantation has been the mainstay of treatment for thalassemia. In a group of patients with specific characteristics evaluated by initial risk assessment, the prediction of transplant success can reach over 90%. Several new regimens have been evaluated to reduce treatment-related morbidity and mortality. Healthcare providers prioritize monitoring records and guidelines for treating infection or regimen-related toxicity after transplantation in these patients, particularly in high-risk cases. Young patients with confirmed thalassemia who are transplanted with donor stem cells with matching levels of human leucocyte antigen (HLA) proteins have a very high likelihood of achieving remission, with a mortality rate of less than 10% and minimal morbidity. Event-free survival rates are 80 – 90% for hemochromatosis [4,5]. In contrast, event-free survival in adult patients with thalassemia major undergoing bone marrow transplantation is less than 70%. A major problem in developing stem cell transplantation therapy in young patients with thalassemia is that HLA-matched stem cells are often unavailable [5].
Treatment of thalassemia with umbilical cord blood stem cells
The outcomes of umbilical cord blood transplantation to treat thalassemia are now approaching those of conventional bone marrow transplantation, with a disease-free survival rate of about 90%. The major benefit of cord blood stem cell transplantation comes from the use of unrelated transplant sources stored in cord blood banks. Transplanting umbilical cord blood stem cells into a patient from an unrelated donor is feasible. However, before transplanting umbilical cord blood stem cells, patients have to take immunosuppression medicine. With transplantation, patients’ life expectancy can reach 50 years or more [6,7].
Compared to stem cell transplantation from bone marrow or peripheral blood, stem cell transplantation from umbilical cord blood offers significant advantages, including a higher ability to create blood cells, which in laboratory tests shows that umbilical cord blood stem cells survive longer in culture with superior in vitro proliferation ability [8] and higher in vivo response potential [9]. In addition, during stem cell transplantation, the level of HLA matching between donor and recipient is less stringent than with bone marrow or peripheral blood stem cells, clinically affecting the incidence and severity of the graft-versus-host disease (GVHD) is relatively low, even in the presence of low HLA mismatch. The rapid availability of cord blood units being stored under incubator conditions, the safety of cell collection, and the control of the risk of transmission of infections and infectious diseases is low or does not make cord blood transplantation a viable alternative, especially for ethnic minority patients in developing countries. In Vietnam, there are several medical facilities that can perform stem cell transplantation from umbilical cord blood to treat thalassemia, such as the Central Blood Transfusion Hematology Hospital and the Ho Chi Minh City Blood Transfusion and Hematology Hospital. In 2020, Vietnam had a typical case of thalassemia cured, thanks to umbilical cord stem cell transplantation. Specifically, a boy with thalassemia received a hematopoietic stem cell transplant from his sister’s umbilical cord blood. The transplant was successful, and the boy no longer needed regular monthly blood transfusions (according to statistics from Vietnamese health – https://ytvn.vn/).
Future perspective
Today, with the increased number of umbilical cord blood stem cell donations, more patients can access curative umbilical cord blood stem cell transplant therapy. However, these alternative donor sources still come with their own challenges, and significant improvements are needed before they can be considered the standard of care. Current recommendations for cord blood stem cell transplantation in treating disease suggest using units containing at least 3.5x107TNC/kg recipient body weight before cryopreservation and with less than two HLA mismatches. The mean numbers of TNC and CD34+ cells infused were 7.8×107/kg (range 2.8–14.7×107/kg) and 4.0×105/kg (range 1.7–19.9×105/kg), respectively [10]. A better understanding of the mechanisms and risk factors leading to graft failure can further optimize the donor selection process, avoiding donor units with HLA mismatches leading to transplant rejection. Different approaches are being explored to overcome the cell dose limitation, including multi-unit co-transplantation, direct intraosseous injection of umbilical cord blood stem cells, or intraosseous hematopoietic stem cell proliferation ex vivo with stimulating agents [11,12,13]. Based on the existing database, umbilical cord blood stem cell transplantation from unrelated sources seems to still be an effective method in the future for thalassemia major, although it is still. Clinical trials are needed to discover specific treatment regimens that help increase graft growth and improve the patient’s quality of life.
References:
- Kattamis, Antonis, Janet L. Kwiatkowski, and Yesim Aydinok. “Thalassaemia.” The Lancet(2022).
- Gao, Jie, and Wenjun Liu. “Advances in Screening of Thalassaemia.” Clinica Chimica Acta(2022).
- Mathews, Vikram. “Allogeneic stem cell transplantation for thalassemia major.” Regenerative Medicine: Laboratory to Clinic(2017): 343-357.
- Krishnamurti, Lakshmanan, H. Franklin Bunn, Andrea M. Williams, and Jakub Tolar. “Hematopoietic cell transplantation for hemoglobinopathies.” Current problems in pediatric and adolescent health care38, no. 1 (2008): 6-18.
- Pinto, Fernando O., and Irene Roberts. “Cord blood stem cell transplantation for haemoglobinopathies.” British journal of haematology141, no. 3 (2008): 309-324.
- Boncimino, Agata, Alice Bertaina, and Franco Locatelli. “Cord blood transplantation in patients with hemoglobinopathies.” Transfusion and Apheresis Science42, no. 3 (2010): 277-281.
- Boncimino, Agata, Alice Bertaina, and Franco Locatelli. “Cord blood transplantation in patients with hemoglobinopathies.” Transfusion and Apheresis Science42, no. 3 (2010): 277-281.
- Lu, Li, Mang Xiao, Rong-Nian Shen, Susan Grigsby, and Hal E. Broxmeyer. “Enrichment, characterization, and responsiveness of single primitive CD34 human umbilical cord blood hematopoietic progenitors with high proliferative and replating potential.” (1993): 41-48.
- Mayani, Hector, and Peter M. Lansdorp. “Biology of human umbilical cord blood-derived hematopoietic stem/progenitor cells.” Stem cells16, no. 3 (1998): 153-165.
- Jaing, T. H., I. J. Hung, C. P. Yang, S. H. Chen, H. T. Chung, P. K. Tsay, and Y. C. Wen. “Unrelated cord blood transplantation for thalassaemia: a single-institution experience of 35 patients.” Bone marrow transplantation47, no. 1 (2012): 33-39.
- Barker, J. N., D. J. Weisdorf, and J. E. Wagner. “Creation of a double chimera after the transplantation of umbilical-cord blood from two partially matched unrelated donors.” New England Journal of Medicine344, no. 24 (2001): 1870-1871.
- Barker, Juliet N., Daniel J. Weisdorf, Todd E. DeFor, Bruce R. Blazar, Philip B. McGlave, Jeffrey S. Miller, Catherine M. Verfaillie, and John E. Wagner. “Transplantation of 2 partially HLA-matched umbilical cord blood units to enhance engraftment in adults with hematologic malignancy.” Blood105, no. 3 (2005): 1343-1347.
- Stiff, Patrick J., Pau Montesinos, Tony Peled, Efrat Landau, Noga Rosenheimer, Julie Mandel, Nira Hasson et al. “StemEx®(copper chelation based) ex vivo expanded umbilical cord blood stem cell transplantation (UCBT) accelerates engraftment and improves 100 day survival in myeloablated patients compared to a registry cohort undergoing double unit UCBT: results of a multicenter study of 101 patients with hematologic malignancies.” (2013): 295-295.
