The application of probiotics in supporting the treatment of infertility in women
Infertility is a common condition that affects approximately 186 million people worldwide (1). Researchers have studied numerous causes of infertility, with age being considered a significant factor influencing both male and female infertility as well as reproductive disorders (2). Besides acute, chronic, or infectious diseases, environmental exposure, occupations, lifestyles, and genetic conditions can also impact the fertilization process. Individuals suffering from infertility or reproductive disorders often resort to assisted reproductive techniques such as in vitro fertilization (IVF) (3).
Infertility significantly affects one’s life, particularly in the context of family relationships. It can lead to societal issues, including illegal practices such as surrogacy and child trafficking. In recent years, several studies have indicated that the microbiome plays a crucial role in treating infertility and contributes to improving the success rates of intervention methods, like IVF (3).
- Causes of Infertility in Women
One of the most common factors leading to vaginal inflammation is the bacterium Ureaplasma parvum (13). As a member of the mycoplasma family, Ureaplasma belongs to the smallest self-replicating microorganisms and parasites in humans, simultaneously being the most pathogenic bacteria in the human genital tract (14). Other causes include:
Uterine Lining: The uterine lining, where the fertilized embryo attaches and develops during pregnancy, can be a factor. If the uterine lining does not thicken or support successful fertilization, it means that even if fertilization occurs, the embryo cannot implant, leading to infertility. Egg Chamber Quality: The quality of the ovarian follicles also affects the development and maturation of eggs. If the eggs do not mature and release as usual, and if the egg chamber cannot rupture, the ovulation process cannot take place, resulting in unsuccessful fertilization and infertility.
Cervical Mucus: Cervical mucus aids in guiding sperm towards the egg during ovulation. If the cervical mucus is too thick or contains certain components, sperm may struggle to pass through the cervix and vagina to reach the male’s uterus, hindering the fertilization process.
- The Relationship Between Female Infertility and Lactobacilli Microorganisms
In the female reproductive tract, the presence and activity of Lactobacilli microorganisms are closely related to vaginal health in women of reproductive age (4,5). Specifically, certain types of Lactobacilli, predominantly Lactobacillus crispatus, Lactobacillus gasseri, Lactobacillus iners, and Lactobacillus jensenii, are found in healthy and fertile women. These Lactobacillus strains produce lactic acid, creating an acidic environment with a pH of less than 4.5. Therefore, they provide a highly protective environment, acting as a barrier to prevent the invasion of pathogens and other disease-causing agents into the reproductive tract (6). Additionally, Lactobacillus species also produce bacteriocins, a type of antibacterial substance that inhibits the growth of unwanted species, such as Klebsiella, Staphylococcus aureus, Escherichia coli, or Enterococcus faecalis (7).
Furthermore, a higher abundance of Lactobacilli creates conditions conducive to better reproductive outcomes for women (8,9). A reduction in the number of Lactobacilli is associated with vaginal inflammation and infections of the vaginal tract (10,11), demonstrating the crucial role of Lactobacilli in women’s reproductive health. Vaginal inflammation and infections of the vaginal tract can impact fertility and pose a risk for inflammation of the membranes, preterm rupture of membranes, and preterm birth in pregnant women (12).
- Testing and Treatment
To investigate the impact of probiotics on supporting the treatment of infertility in women, 80 primary or secondary infertility patients were enrolled in a study. Forty patients were assigned to receive probiotic treatment, while the other 40 patients did not receive probiotics. Women in the treatment group were administered a daily 2g packet of probiotics supplementing specific strains of Lactobacillus. Patients in the control group did not receive any probiotic supplements. Then, the researchers obtained vaginal fluid samples on the 20th day of the menstrual cycle and four weeks later, around the 20th day of the subsequent cycle. Subsequently, researchers analyzed the rRNA genes of these vaginal samples (15).
After the use of probiotics, there were no discernible health impacts on the patients, despite variations in age, body indices, and other health conditions. Results indicated a positive effect of the probiotics used on the patients. Researchers identified three strains of microorganisms (Lactobacillus crispatus, Lactobacillus iners, and Lactobacillus gasseri) that positively limited the growth of Ureaplasma parvum. When comparing infertility patients who were treated with specific Lactobacillus strains to those who received no intervention, the treatment group showed a significantly lower development ratio of Ureaplasma parvum. The study demonstrated the influence of Lactobacilli in supporting female infertility by reducing and restricting the growth of Ureaplasma parvum (15).
- Conclusion
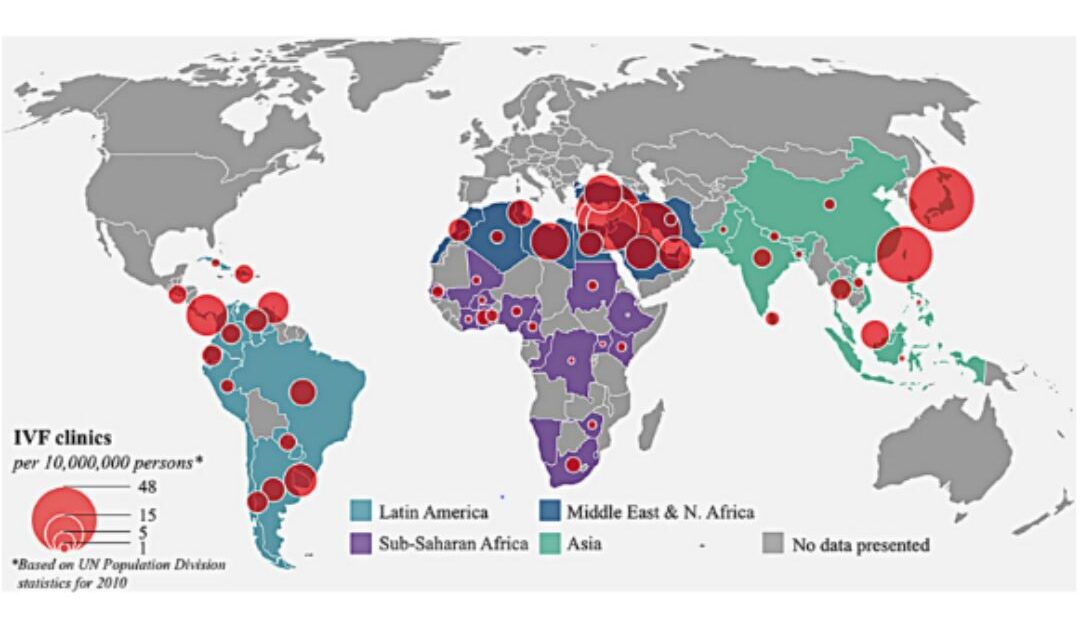
Up to the present, infertility, both in general and specifically in women, remains a prevalent global health issue (Figure 1) (1). Individuals affected by this condition still encounter numerous challenges in treatment due to high costs and complex therapeutic interventions. Therefore, it is crucial to explore treatment approaches, particularly utilizing probiotics, to support and address female infertility. However, further in-depth research is still necessary to better understand the role of microorganisms in infertility treatment for future advancements.
References:
- Inhorn, M. C., & Patrizio, P. (2015). Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century. Human reproduction update, 21(4), 411-426.
- Cunningham, J. (2017). Infertility: A primer for primary care providers. Journal of the American Academy of PAs, 30(9), 19-25.
- Sirota, I., Zarek, S. M., & Segars, J. H. (2014, January). Potential influence of the microbiome on infertility and assisted reproductive technology. In Seminars in reproductive medicine (Vol. 32, No. 01, pp. 035-042). Thieme Medical Publishers.
- Moreno, I., Codoñer, F. M., Vilella, F., Valbuena, D., Martinez-Blanch, J. F., Jimenez-Almazán, J., … & Simon, C. (2016). Evidence that the endometrial microbiota has an effect on implantation success or failure. American journal of obstetrics and gynecology, 215(6), 684-703.
- Miles, S. M., Hardy, B. L., & Merrell, D. S. (2017). Investigation of the microbiota of the reproductive tract in women undergoing a total hysterectomy and bilateral salpingo-oopherectomy. Fertility and sterility, 107(3), 813-820.
- Linhares, I. M., Summers, P. R., Larsen, B., Giraldo, P. C., & Witkin, S. S. (2011). Contemporary perspectives on vaginal pH and lactobacilli. American journal of obstetrics and gynecology, 204(2), 120-e1.
- Stoyancheva, G., Marzotto, M., Dellaglio, F., & Torriani, S. (2014). Bacteriocin production and gene sequencing analysis from vaginal Lactobacillus strains. Archives of microbiology, 196, 645-653.
- Egbase, P. E., Al-Sharhan, M., Al-Othman, S., Al-Mutawa, M., Udo, E. E., & Grudzinskas, J. G. (1996). Fertilization and early embryology: Incidence of microbial growth from the tip of the embryo transfer catheter after embryo transfer in relation to clinical pregnancy rate following in-vitro fertilization and embryo transfer. Human Reproduction, 11(8), 1687-1689.
- Salim, R., Ben-Shlomo, I., Colodner, R., Keness, Y., & Shalev, E. (2002). Bacterial colonization of the uterine cervix and success rate in assisted reproduction: results of a prospective survey. Human Reproduction, 17(2), 337-340.
- Moreno, I., & Franasiak, J. M. (2017). Endometrial microbiota—new player in town. Fertility and sterility, 108(1), 32-39.
- Kyono, K., Hashimoto, T., Nagai, Y., & Sakuraba, Y. (2018). Analysis of endometrial microbiota by 16S ribosomal RNA gene sequencing among infertile patients: a single‐center pilot study. Reproductive Medicine and Biology, 17(3), 297-306.
- Redelinghuys, M. J., Geldenhuys, J., Jung, H., & Kock, M. M. (2020). Bacterial vaginosis: current diagnostic avenues and future opportunities. Frontiers in cellular and infection microbiology, 10, 354.
- Haggerty, C. L., Totten, P. A., Ferris, M., Martin, D. H., Hoferka, S., Astete, S. G., … & Ness, R. B. (2009). Clinical characteristics of bacterial vaginosis among women testing positive for fastidious bacteria. Sexually transmitted infections, 85(4), 242-248.
- Cassell, G. H., Waites, K. B., Watson, H. L., Crouse, D. T., & Harasawa, R. (1993). Ureaplasma urealyticum intrauterine infection: role in prematurity and disease in newborns. Clinical microbiology reviews, 6(1), 69-87.
- Schenk, M., Grumet, L., Sternat, J., Reinschissler, N., & Weiss, G. (2021). Effect of probiotics on vaginal Ureaplasma parvum in women suffering from unexplained infertility. Reproductive BioMedicine Online, 43(3), 503-514.
